Vaccination FAQs
Updated December 29, 2022
VACCINE CLINIC WED JAN 18 AT PORTSMOUTH SENIOR ACTIVITY CENTER, 9 AM–3 PM – Free and open to the public, 125 Cottage Street. Pfizer and Moderna boosters as well as initial series and vaccines for children available.
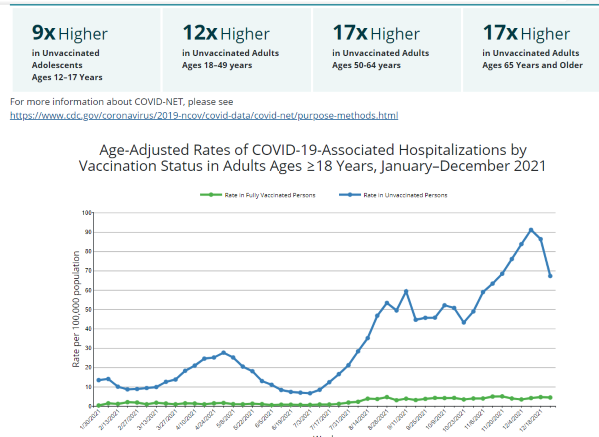
CDC research conducted through Dec 2021 demonstrates that those who are not vaccinated have significantly higher levels of severe illness and hospitalization from COVID-19.
Go to the interactive website to find a convenient vaccination site.
In August 2022, NH DHHS provided these updated charts showing the appropriate vaccination schedules for those age 6 mos and older and for the immunocompromised (second graph, below):

J&J VACCINE
On May 5, 2022, the FDA limited who can receive Johnson & Johnson’s COVID-19 vaccine due to the ongoing risk of rare but serious blood clots. The shot should only be given to adults who cannot receive a different vaccine or specifically request the J&J.
Those who are severely immunocompromised or have other concerns related to age or medical condition have slightly different vaccination recommendations. Check with your healthcare provider.
To learn more and find vaccination sites go to Vaccines.gov
On May 5, 2022, the FDA limited who can receive Johnson & Johnson’s COVID-19 vaccine due to the ongoing risk of rare but serious blood clots. The shot should only be given to adults who cannot receive a different vaccine or specifically request J& J’s vaccine. FDA’s vaccine chief Dr. Peter Marks said the agency decided to restrict the vaccine after taking another look at the data on the risks of life-threatening blood clots and concluding that they are limited to J& J’s vaccine. The problem occurs in the first two weeks after vaccination. Under the new FDA instructions, J& J’s vaccine could still be given to people who had a severe allergic reaction to one of the other vaccines and can’t receive an additional dose. J& J’s shot could also be an option for people who refuse to receive the mRNA vaccines from Pfizer and Moderna, and therefore would otherwise remain unvaccinated.
All three COVID-19 vaccines with FDA Emergency Use Authorization are now available in NH and are available, free, during the mobile clinics and at the vaccination sites listed below.
You can also text your zip code to 438829 to receive a listing of all the sites in your area that have the vaccine. The text that comes back also asks if the individual needs a ride and if so, the ride is set up for them. If needed, free childcare is made available while getting vaccinated (just send a reply text with “CARE” ). There is also a phone number listed: 1-800-232-0233 to get more help and/or info.
BOOSTERS FOR HOMEBOUND INDIVIDUALS Call On-Site Medical Services, the company contracted by NH to provide homebound boosters, at 603.826.6500 to make an appointment, or go to their website.
If you have language issues that prevent you from understanding registration instructions for the COVID-19 vaccine, please contact Kim McNamara at the Portsmouth Health Department or call (603) 610-7273. If you get voicemail, please be sure to leave a message.
FALL BOOSTERS
The Centers for Disease Control and Prevention have said that a national survey found that 72 percent of respondents said they were likely to receive an updated booster. But getting people vaccinated requires making the boosters easily accessible and making sure people know about their benefits.
How is the new booster different from my original COVID-19 vaccination (and booster)?
This is the first time, the United States is rolling out Covid vaccines updated to match variants that are currently dominant, as well as the original strain. This will provide a better response to the most threatening variants today but probably to future variants, too, because when the immune system faces different versions of the same virus it generates broader protections overall. In addition to decreasing the likelihood of infection and severe illness and help reduce transmission of the virus; it could also decrease the likelihood of developing long Covid.
I’m young, healthy, vaccinated and had an uneventful breakthrough infection. Why should I get the booster?
You might want a booster to avoid getting sick or risking of long Covid. But vaccines dampen spread, and boosters can further reduce transmission of the disease, including by reducing infections in the first place, and thus help protect especially the more vulnerable.
Don’t I have enough protection from previous doses or past infections?
Many who did not get the previous booster, and many who don’t plan to get the updated one, that they did not believe the boosters to be effective — a claim that is routinely made because Omicron caused a lot of breakthrough infections among the vaccinated. In Canada and many European countries where two-thirds of adults got boosters. the cumulative death and illness tolls from the Omicron wave are sharply lower than those of the United States, where only about a third of eligible adults had gotten boosters. The United States has had a death rate 80 percent greater than Canada’s from the Omicron wave
Why bother with one more shot?
About 68 percent of Americans have had two initial vaccination shots, some have had booster shots, and got some level of immunity from an Omicron infection. Protection against severe disease remains fairly strong. But variants evolved that evaded the antibody protection generated by earlier vaccines. The new boosters can greatly decrease that evasion by better training both antibodies and memory cells. Being exposed to different versions of the virus further deepens and broadens the kind of antibodies that get generated, including ones that can work against future variants. Where can I get the new booster?
Your primary care provider and most local pharmacies are able to provide booster vaccinations (most by appointment). Find a location most convenient to you at vaccines.gov As of September 19, there were 50 free vaccination locations listed within the region for Portsmouth’s zipcode 03801.
For the latest CDC information about the COVID-19 vaccine, including "Key Things to Know," click here.
For more "Answers to All Your Questions About Getting Vaccinated for COVID-19," click here.
For "I've been vaccinated, now what?" FAQs, click here.
What about booster shots of COVID-19 vaccines?
On November 19, 2021, CDC issued the following statement: For individuals received a Pfizer-BioNTech or Moderna COVID-19 vaccine are eligible for a booster shot at 6 months or more after their initial series. For the nearly 15 million people who got the Johnson & Johnson COVID-19 vaccine, booster shots are also recommended for those who are 18 and older and who were vaccinated two or more months ago.
There are now booster recommendations for all three available COVID-19 vaccines in the United States. Eligible individuals may choose which vaccine they receive as a booster dose. Some people may have a preference for the vaccine type that they originally received and others, may prefer to get a different booster. CDC’s recommendations now allow for this type of mix and match dosing for booster shots.
Does the discussion about vaccine "boosters" mean that the vaccines are not effective?
No. All three COVID-19 vaccines protect against getting COVID-19 if exposed and reduce the severity of the infection and the risk of hospitalization or death if a vaccinated person becomes infected. The most recent research suggests that those who do not have strong immune systems (those over 65 and immunocompromised people) can benefit by treating mRNA vaccinations as a three-dose series, rather than the two-doses. The mRNA vaccines can also be modified to protect better against emerging variants, so that "boosters" can protect against new strains, the same way annual "flu shots" (designed for the anticipated strain of flu) do.
- Studies so far indicate that boosters do “boost” immunity from COVID-19 secured from primary full vaccination and natural immunity from previous infection.
- Primary vaccination does wane. Boosters provide a bump to immunity.
- CDC says everyone over 18 should receive a booster; those 16-17 “may” receive.
- DPHS says everyone over 5 should receive the primary vaccination and everyone over 16 should receive the booster.
Summary of early Omicron variant studies:
- Variant appears to be more infectious.
- Substantially decreased (10-40x less effective) antibody immunity from vaccination and/or previous infection.
- 2-dose mRNA vaccine is 30-40% effective in preventing COVID-19 from Omicron.
- Booster dose increases antibody immunity to 75% (still lower than vaccine effectiveness against other variants.)

How much will it cost to get the vaccine?
Nothing. Tax dollars funded the vaccine research and production so the vaccine you receive is free.
Is the vaccination painful?
The vaccination involves an injection into your upper arm with a thin needle. The shot itself will feel the same as other vaccinations you have received.
I lost my proof-of-vaccination card. Now what?
All vaccination records are kept on file in the CDC National Health Interview Survey (NHIS) system. NH DHHS advises that you can replace a lost vaccination card in either of two ways:
- Download and complete this vaccination card replacement request form . Note that the completed form MUST BE NOTARIZED before sending it back to NH DHHS.
- If your healthcare provider has access to the NHIIS, ask him/her to print out the record directly from NHIIS.
---------------------------------------------------------
FACTS ABOUT THE COVID-19 VACCINES
Studies show that COVID-19 vaccines are safe and very effective at preventing hospitalization and death from COVID-19. Now that there are authorized and recommended COVID-19 vaccines in the United States, accurate vaccine information is critical. COVID-19 vaccinations are critical to stopping the pandemic. None of the COVID-19 vaccines contain the live virus that causes COVID-19 so a COVID-19 vaccination cannot give you COVID-19. While more COVID-19 vaccines are being developed as quickly as possible, routine processes and procedures remain in place to ensure the safety of any vaccine that is authorized or approved for use. Safety is a top priority, and there are many reasons to get vaccinated
What is a vaccine?
A vaccine is a substance used to stimulate the production of antibodies and provide immunity against one or several diseases without causing the disease. Vaccines are in a category of substances known as antigens.
What are antigens?
An antigen is a substance foreign to the body that, when recognized by the body’s immune system, brings about a response to rid the body of the antigen and either prevent or minimize illness. These responses, called immune responses, include directly “killing” the antigen, bringing about the production of antibodies to neutralize the antigen, and producing “memory cells” so that if the antigen is detected in the future it can be destroyed by the immune system.
What are the different types of vaccines for COVID-19?
Several different pharmaceutical companies started working to develop a COVID-19 vaccine in the spring of 2020. FDA’s Center for Biologics Evaluation and Research [CBER] ensures that FDA’s rigorous scientific and regulatory processes are followed by those who pursue the development of new vaccines. The vaccines that have been made public include the mRNA vaccines made by Pfizer and Moderna. The Adenoviral vaccine made by Johnson and Johnson was approved on February 28 and reaffirmed on April 23.
What is an mRNA vaccine?
This type of vaccine uses viral messenger RNA (mRNA) to teach the immune system to recognize viruses as antigens. mRNA, found in all cells, provides cells with instructions on how to make proteins (among other functions). In the case of activating the immune system, the mRNA instructions cause the cell to make a protein that is very similar to the virus or one of its parts. Once this protein is made and “displayed” on a cell surface the body then recognizes this altered cell as foreign (an “antigen”) and begins to produce antibodies against the antigen. This technology DOES NOT use a live or weakened form of the virus, nor does it affect the nucleus or DNA of the cell. These mRNA vaccines do not and cannot infect those who receive them with COVID-19. While mRNA vaccines represent a new technology, using mRNA to produce antibodies is not new; this approach has been studied in laboratories for many years.
How do the COVID-19 mRNA vaccines work?
The COVID-19 mRNA vaccine is first injected into a muscle in your upper arm. The vaccine then enters nearby cells and instructs them to make a piece of the COVID-19 “spike protein” that plays a role in anchoring the virus to respiratory and other body tissues. Once the mRNA instruction is received by your cells, those cells start manufacturing the spike protein and display it on their surface. The presence of the “foreign” spike protein on the surface of the cell causes your body to produce antibodies against the spike protein. Should you become exposed to the virus, these antibodies will recognize the COVID-19 spike protein and fight the virus or minimize its infectiousness.
What is an adenoviral vaccine?
An adenoviral vaccine uses an adenovirus -- common viruses that typically cause colds or flu-like symptoms -- to activate an immune response. This technology is the basis for many vaccines that are already in widespread use. These vaccines insert a gene that codes for a protein into an unrelated adenovirus that has been modified and rendered harmless. Once rendered harmless this adenovirus with the inserted gene will not and cannot infect anyone with COVID-19. Once administered in the vaccination, the adenovirus attaches to a cell surface, moves into the cell, enters the cell nucleus, and incorporates into the cell DNA. This causes the cell nucleus to “read” the inserted gene and instructs its natural mRNA to begin making the protein instructed by the inserted gene. The Johnson and Johnson vaccine is an adenoviral vaccine.
How do the adenoviral COVID-19 vaccines work?
The gene for the coronavirus “spike protein” is inserted into an adenovirus that has been modified to render it harmless (it cannot cause COVID-19).Once administered into a muscle in the upper arm this modified adenovirus enters a cell, travels to the nucleus, and inserts the gene for making the spike protein into the host cell DNA. The host cell “reads” the gene for the COVID-19 spike protein and copies the instructions for making the spike protein onto natural mRNA. The mRNA then directs the cell’s protein-building structures to produce the COVID-19 spike protein. The manufactured spike protein travels to the surface of the cell where it is recognized by the immune system as “foreign” and starts producing antibodies against the spike protein. Should you become exposed to the virus, these antibodies will recognize the COVID-19 spike protein and eradicate the virus or minimize its infectiousness.
How are the two vaccines that use mRNA different?
The Pfizer and Moderna mRNA vaccines are composed of mRNA containing the instructions for making the COVID-19 spike protein so that once the vaccine is taken into a cell the protein building instructions are already in place and spike proteins can be made by the cell protein building structures.
The adenoviral vaccines contain the instructions for building the spike protein on a gene that has been incorporated into a modified adenovirus. Once this vaccine enters the cell it travels to the cell nucleus where it inserts the gene for making the spike protein into the cell DNA. The cell DNA then transfers these instructions to its own mRNA. This mRNA then leaves the cell nucleus and travels to the cellular structures that build the spike protein.
Is there any new information about how well the mRNA vaccines work?
The New England Journal of Medicine has reported findings from a study of 3,975 participants -- those who were partially or fully vaccinated as well as unvaccinated -- who became infected with COVID-19.
There were 156 cases of COVID-19 among the unvaccinated group. 11 among partially vaccinated (81% effectiveness). 5 among fully vaccinated (91% effectiveness.
The vaccinated group who had breakthrough infection experienced the following benefits compared to the unvaccinated:
- 40% lower viral shedding (i.e. less-contagious)
- 6 fewer days of identified infection
- 60% lower risk of spreading infection after 1 week
- 58% lower risk of fever (just this symptom was studied)
- 6 fewer days of symptoms
- 2.3 fewer days "sick in bed"
For more information including drawings showing how adenoviral and mRNA vaccines work, visit:
New York Times, How the Moderna Vaccine Works
New York Times, How the AstraZeneca Vaccine Works
USA Today, How New RNA Technology Was Used to Create COVID-19 Vaccines

For more "myth-buster" facts from the CDC about the COVID-19 vaccines, click here.
Does it make a difference which vaccine I receive?
No. The FDA, CDC and NH DHHS stress that all three vaccines are safe and highly effective for preventing severe illness, hospitalization and death. Residents should take the first opportunity offered to be vaccinated.
What about the problems from the Johnson & Johnson (Janssen) vaccine in April 2021?
After a few cases of rare blood clotting complications, J & J vaccine use was temporarily halted so that experts at the FDA and CDC could investigate and develop treatment guidelines for this extremely rare complication. On April 23 the guidelines were finalized and along with the recommendation to resume use of the J&J vaccine as safe and effective. The committee also encouraged that those choosing the J&J vaccine be aware that there is an extremely low risk of developing a rare side-effect called TTS (Thrombosis-Thrombocytopenia Syndrome) that causes both blood clotting and decreased platelets in the blood.
- This rare side-effect was observed in 15 cases out of 8.9 million J&J doses administered in the US.
- Of those cases, 13 were women between 18 and 49 (a rate of 7 in 1 million).
- FDA guidance is that J&J is safe and effective for that population group
- Members of the group can choose one of the other two vaccines if they prefer.
Side-effects that might suggest TTS include headaches that occur within 6 to 15 days after vaccination – NOT within 2-3 days as headaches are seen as a normal side-effect from receiving the J&J vaccine.
Women who have a history of the blood-clotting syndrome HIT should consider either Moderna or Pfizer vaccines.
Those who are on an aspirin or other anticoagulant regimen may safely receive the J&J vaccine; but otherwise, people should not take aspirin or other anticoagulant before any vaccine.
Can I get one dose of one of the vaccines and the second dose of the other 2-dose vaccine?
No – while both the Pfizer and Moderna mRNA vaccines require two doses, the manufacturing process of each vaccine was different and proprietary for each company. Since the vaccines differ in composition, storage, and time between doses, people must get the same vaccine for both doses. However, you can 'mix and match' vaccines for booster shots. CDC even recommends that those who received the J&J vaccine receive an mRNA vaccine as a booster.
What if I miss the second vaccination?
The two currently approved vaccines are: 21 days between shots for Pfizer and 28 days between shots for Moderna. The card you receive after the first vaccination will list which vaccine you received and when your second dose is scheduled.
Should you miss your appointment or need to reschedule for any reason, be sure to get the second shot as soon as possible to ensure the benefit of full immunity. Regarding timing in between the first and second vaccine: those who are concerned they have not been able to schedule their second vaccine within the 21 or 28 day interval should know that these intervals are a minimum amount of time necessary between each dose. No maximum interval has been established for the second dose. NH DHHS and the CDC feel quite confident that there is the same amount of protection even if the time interval between the first and second dose is longer than 21 or 28 days.
SIDE EFFECTS

Is the vaccination painful?
The vaccination involves an injection into your upper arm with a thin needle. The shot itself will feel the same as other vaccinations you have received.
What are the side effects?
All vaccine trial participants reported minor side effects common to many vaccinations including a sore arm or feeling poorly, fatigue, or tired for a day or two after the shot. Other reported side effects included headache, fever and chills, and other muscle aches/pain primarily after the 2nd shot that lasted a day or two. Some vaccine trial participants treated these side effects with pain medication, but you are advised not to take pain medication before receiving Dose 2, in anticipation of side effects, as that would diminish the effectiveness of the vaccine. Side effects show that the vaccination is working -- your body is responding. The percentage of participants experiencing these side effects depend on the vaccine administered. For specific percentages detailed in the report, click here.
There have been isolated reports of more severe side effects including allergic reactions. You should discuss getting the vaccine with your health care provider to determine if you are at risk for a more severe reaction. You will also be asked to stay for 15-30 minutes after receiving the vaccine to monitor for any serious side effect and to receive the vaccination in a place capable of providing prompt emergency care.
There have been isolated reports of a rare blood clotting disorder associated with the J & J vaccine. Refer to the earlier question for more information.
What is known about the long term complications of COVID-19 What is a “COVID-19 Long Hauler?” Does the vaccine help prevent this complication?
Significant numbers of people continue to experience troublesome symptoms for 3 or more months following initial COVID-19 infection. Sometimes the symptoms are new and sometimes they continue to linger beyond the usual recovery period. “COVID-19 long hauler” is the term used to describe this phenomenon, which can be quite debilitating. The medical term is Post-Acute Sequelae of SARS-CoV-2 infection or PASC. The best way to prevent long term complications is to avoid infection in the first place by being vaccinated and following the guidelines for mask wearing, physical distancing, and handwashing.
What should I do if I have a bad reaction to the vaccine?
If you have a bad reaction, you should notify your primary care provider immediately. If you are having trouble breathing, notice any sudden swelling (especially of your face or tongue), or feel faint after you have received the vaccine and left the facility, call 911 for immediate emergency care.
The CDC and FDA encourage the public to report possible side effects (called “adverse events”) to the Vaccine Adverse Event Reporting System (VAERS)external icon external icon. This national system collects data to look for adverse events that are unexpected, appear to happen more often than expected, or have unusual patterns of occurrence. Reports to VAERS help the CDC monitor the safety of vaccines. Safety is a top priority.
The CDC is also implementing a new smartphone-based tool called “v-safe” to check-in on people’s health after they receive a COVID-19 vaccine. When you receive your vaccine, you should also receive a v-safe information sheet telling you how to enroll in v-safe. If you enroll, you will receive regular text messages directing you to surveys where you can report any problems or adverse reactions you have after receiving a COVID-19 vaccine.
I have a history of allergies – should I get the vaccine?
In all cases, if you have any concerns or questions about the vaccine, you should ask your health care provider. Since its public rollout both vaccines have been associated with an immediate allergic reaction in a very small number of people. These reactions have occurred within the first 30 minutes after receiving the shot; for this reason, those with severe anaphylaxis to anything (drug, food, insect bites, etc. should be informed of the risk and monitored for 30 minutes rather than 15 minutes after vaccination to be sure you do not have a serious allergic reaction.
Right now, it is highly recommended that persons who have had an anaphylactic reaction to any drug, food or other vaccine NOT receive the vaccine. Both vaccines have only one contraindication: known history of a severe allergic reaction to any component of the vaccine. The DHHS guidance says those with severe anaphylaxis to anything, should be informed of risk and monitored for 30 minutes rather than 15. It does not say they shouldn't get the vaccine.
If I have had COVID-19 do I need to get a vaccination?
Yes! According to the CDC, even people who have already gotten sick with COVID-19 may benefit from the vaccine. If you were treated for COVID-19 symptoms with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID-19 vaccine. Talk to your doctor if you are unsure what treatments you received or if you have more questions about getting a COVID-19 vaccine.
COVID-19 can lead to serious illness and long-term complications, even in younger people and those without underlying medical conditions. It is possible for someone who has already had COVID-19 to be re-infected, though this is not common.
It is not yet known how long natural immunity to COVID-19 lasts or if the strength or duration of natural immunity varies based on the severity of the initial illness.
If I received monoclonal antibodies or convalescent plasma to treat COVID-19 should I get a vaccination?
Based on the research on these therapies, as well as evidence suggesting that reinfection is uncommon in the 90 days after initial infection, vaccination should be deferred for at least 90 days, as a precautionary measure until additional information becomes available, to avoid potential interference of the antibody therapy with vaccine-induced immune responses.
I have heard that some people develop COVID-19 after getting their first shot. if this happens should I reschedule my second shot?
Full immunity to COVID-19 after receiving the vaccination takes time to develop. Early studies of the Moderna and Pfizer vaccines reported about 50% protection after the first shot. This means that once your immune system began to develop antibodies to COVID-19 you still have a 50-50 chance of contracting the infection after the initial shot. This is one of the reasons it is important to continue to wear a mask, physically distance, and wash your hands frequently, per CDC recommendations.
If you develop COVID-19 after your first shot, you should delay the second shot until you have recovered from the acute illness (if you have symptoms) and have been met the DHHS criteria for ending isolation.
I've heard some people get myocarditis or pericarditis (inflammation of the heart wall or surrounding tissue)?
Two new studies reported by the CDC found that:
Out of 296 million doses there were 1,226 reported cases of myocarditis, or 4 in 1 million doses.
Of those cases:
- Median age = 26
- 58% under age 30.
- 77% males
- Onset occurred 3 days after the vaccine dose.
- 76% occurred after the 2nd dose.
- No deaths
Another study of 484 cases of myocarditis (not all following vaccination):
- Median age = 19 years.
- 90% males
- Onset occurred 2 days after vaccination. 92% developed symptoms within 7 days.
- 96% were hospitalized for chest pain/shortness of breath which resolved after mild clinical monitoring.
- No deaths.
The conclusion is that the benefits of the vaccine (prevention of COVID-19 infection, hospitalization, possible death or Long COVID) far outweigh the very rare and uncommon side effect of myocarditis. CDC strongly recommends that anyone over 12 who is able to be vaccinated should do so.
I’m pregnant and/or breastfeeding – should I get a vaccine?
You should discuss vaccination with the person providing your pregnancy or breastfeeding care, but research has determined that the vaccine is safe and effective for pregnant and breast-feeding women.
I have chronic health problems that put me at higher risk should I get COVID-19, should I get the vaccine?
It is important to discuss with your primary care provider your potential risk should you develop COVID-19 and the benefit you might receive from vaccination. Those with chronic health conditions including asthma, COPD, diabetes, heart disease, and obesity are at higher risk of becoming seriously ill should they contract COVID-19. Persons with pre-existing conditions are more likely to need hospitalization, oxygen support, and sometimes intensive care including a mechanical ventilator. The vaccine trials have included people with pre-existing conditions for exactly this reason; and the vaccines have been demonstrated to be safe in trial participants with pre-existing conditions.
I don’t want to get a vaccine, what other ways can I protect myself from contracting COVID-19?
A good place to start for accurate information on your risks, whether or not you choose to become vaccinated, is with your primary care provider. Your PCP has all the health information you’ve shared available to carefully and thoughtfully help you consider your benefit and risk for vaccination.
Whether you choose to be vaccinated with a COVID-19 vaccine or not, you should continue to follow all recommendations for avoiding infection and if infected, not spreading the infection to others. Those recommendations are often referred to as the 3 C’s: avoid crowded places, contact with infected persons, and closed spaces and, the 3 W’s: Wear a mask, Wash your hands frequently, and Watch your distance—maintaining 6’ apart from others (also called physical distancing).
WHY GET VACCINATED?
A recent survey by the Pew Research Center found that more Americans (60%) say they would probably or definitely get the vaccine when it is available to them – up from the 51% who said so in September. But many Americans still have questions, and these suggestions are offered to help you encourage your families, friends and community members to get the vaccine. Read the full article here.
The vaccine is the key tool for ending the pandemic and relaxing the restraints on "normal" life.
All three vaccines are safe and effective -- and went through full clinical trials before the FDA granted Emergency Use Authorization and they were recommended by the CDC.
AFTER VACCINATION
Once vaccinated how long does it take to be protected?
In general, it takes 14 days after the last vaccine shot to have robust immunity. (Pfizer and Moderna vaccines each require two shots). Before that time, you may have some protection against COVID-19 but it is not possible to predict how protected you are before completing the vaccination schedule.
Once I’m vaccinated, do I still need to wear a mask?
CDC guidance for those who have been vaccinated recommends that residents in areas with “High” or “Severe” Community Transmission rates should consider wearing masks indoors, whether they are vaccinated or not, due to the higher infectiousness of the Delta variant. New research published in the CDC weekly report found that both vaccinated and unvaccinated people can transmit the Delta variant of COVID-19. The CDC’s masking recommendation was updated "to ensure the vaccinated public would not unknowingly transmit virus to others, including their unvaccinated or immunocompromised loved ones." For the latest NH DHHS currently levels of community transmission on the Seacoast, click here.
Infections happen in only a small proportion of people who are fully vaccinated, even with the Delta variant. However, preliminary evidence suggests that fully vaccinated people who do become infected with the Delta variant can spread the virus to others. To reduce their risk of becoming infected with the Delta variant and potentially spreading it to others: CDC recommends that fully vaccinated people:
- Wear a mask in public indoor settings if they are in an area of substantial or high transmission. NOTE: For the latest NH DHHS information on local community transmission levels, click here: https://www.covid19.nh.gov/dashboard/map
- Fully vaccinated people might choose to mask regardless of the level of transmission, particularly if they or someone in their household is immunocompromised or is at increased risk for severe disease, or if someone in their household is unvaccinated. People who are at increased risk for severe disease include older adults and those who have certain medical conditions, such as diabetes, overweight or obesity, and heart conditions.
- Get tested if experiencing COVID-19 symptoms.
- Get tested 3-5 days following a known exposure to someone with suspected or confirmed COVID-19 and wear a mask in public indoor settings for 14 days after exposure or until a negative test result.
Individual businesses and localities are permitted to require masks under the Governor's new "Universal Best Practices" guidance.
If I’m vaccinated, and all my friends and family are vaccinated, can we hang out together without masks?
Yes – BUT: There are four questions to ask if you want to spend time indoors with others, being mindful of their risk:
- Are you vaccinated?
- Is everyone else in the room vaccinated?
- What’s the level of spread in the community?
- Is someone in the room at high risk?
Even if everyone in the room is vaccinated, you need to think about the last two questions. The vaccine gives you about 90-95 percent protection. You also need to think about your odds of coming into contact with the virus. A 5-10 percent risk of infection when the virus is raging is still a significant risk and not low enough when the cases remain high in your community.
The final question — is someone in the room at high risk — is also important. Even if a high-risk person is fully vaccinated, you need to take extra precautions when virus case counts are high in your community. It is important to remember that the vaccine may not be 90-95 percent effective in every single person — an older person or someone with a less efficient immune system might get less protection from the vaccine than a young, healthy person.
RESOURCES
Do you have additional questions about the COVID-19 vaccinations in NH?
Email covidvaccine@dhhs.nh.gov
For more information on the vaccines, visit:
- NY Times, What to Expect When It's Time to Roll Up Your Sleeve: Vaccination FAQs (January 31, 2021)
- NH DHHS: Vaccination FAQs
- CDC: COVID Vaccine Guide to side effects, when it will be out, ingredients (usatoday.com) https://www.cdc.gov/vaccines/COVID-19/index.html
Homebound individuals are being reached by the VNA and other home healthcare providers. But if you do not have a home healthcare provider, and are over 65 or have two qualifying medical issues, call 2-1-1 to schedule a vaccination.
The 211 Hotline remains available, 7 days a week, 6 am to 10 pm.